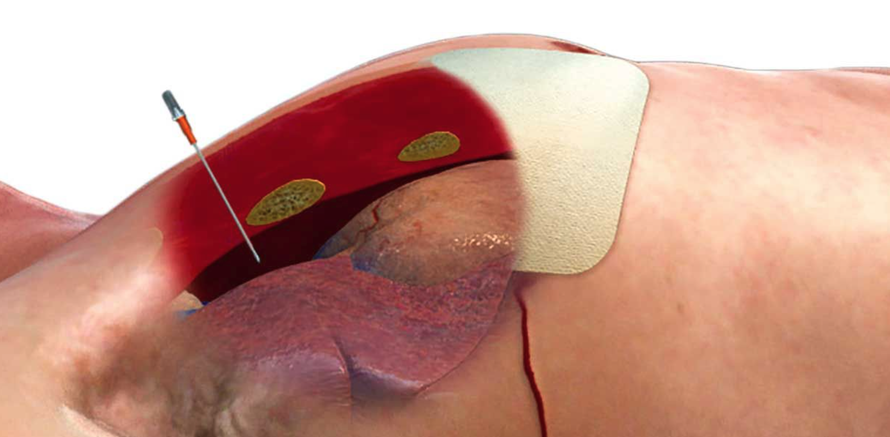
ARS 10G Needle Decompression (10G X 3.25 IN.)
Steeds meer organisaties stappen over van de huidige 14 Gauge naald naar de 10 Gauge versie van Air Release System (ARS) voor de behandeling van een spanningspneumothorax. De ARS 10G versie is qua diameter 60% groter dan de ARS 14G versie, de kans op verstopping is met deze grotere diameter aanzienlijk kleiner. De keuze wordt ook ondersteund door een aantal studies. Hieronder kunt u de samenvattingen lezen!Bigger is better: Comparison of alternative devices for tension hemopneumothorax and pulseless electrical activity in a Yorkshire swine model
Matthew L Leatherman 1, Laura M Fluke, Christian S McEvoy, Douglas M Pokorny, Robert L Ricca, Matthew J Martin, Christopher S Gamble, Travis M PolkAffiliations expand
- PMID: 28885469
- DOI: 10.1097/TA.0000000000001684
Abstract
Background: Tension pneumothorax is a cause of potentially preventable death in prehospital and battlefield settings and 14-gauge angiocatheter (14G AC) decompression remains the current treatment standard, despite its high incidence of failure. Traumatic pneumothorax is often associated with hemothorax, but 14G AC has no proven efficacy for associated hemothorax. We sought to compare the 14G AC to three alternative devices for treatment of tension hemopneumothorax (t-H/PTX) in a positive-pressure ventilation swine model.
Methods: Our tension model was modified to incorporate a persistent air leak and pleural blood. Tension physiology was achieved with escalating carbon dioxide insufflation via transdiaphragmatic trocar, and 10% estimated blood volume was instilled into each chest. Intervention was randomized between 14G AC, 10-gauge angiocatheter (10G AC), modified Veress-type needle (mVN), and 3-mm laparoscopic trocar (LT). After recovery, serial tension-induced pulseless electrical activity (PEA) events were induced and decompressed. Success of rescue, time to rescue, and physiologic data were recorded.
Results: One hundred ninety-five t-H/PTX and 88 PEA events were conducted in 25 swine. Laparoscopic trocar and 10G AC were more successful and had faster median time to rescue for t-H/PTX compared with 14G AC, whereas mVN performed comparably. Following PEA, 14G AC and mVN succeeded at rescue only 50% and 57% of the time, whereas 10G AC and LT had 100% success at return of spontaneous circulation. Time to successful return of circulation following PEA did not differ between devices; however, there was a noticeable difference in the rate of meaningful hemodynamic recovery following PEA favoring LT and 10G AC. There were no significant injuries noted.
Conclusions: While mVN performed comparably to 14G AC, both have unacceptable failure rates. Ten-gauge AC and LT performed superiorly in both t-H/PTX and PEA. We believe there is now ample evidence supporting replacement of the 14G AC with 10G AC in current treatment recommendations.
McEvoy CS, Leatherman ML, Held JM, Fluke LM, Ricca RL, Polk T. 18(4). 18 - 23. (Case Reports)
Abstract
Background: The 14-gauge (14G) angiocatheter (AC) has an unacceptably high failure rate in treatment of tension pneumothorax (tPTX). Little is known regarding the interplay among hemorrhage, hemothorax (HTX), and tPTX. We hypothesized that increased hemorrhage predisposes tension physiology and that needle decompression fails more often with increased HTX. Methods: This is a planned secondary analysis of data from our recent comparison of 14G AC with 10-gauge (10G) AC, modified 14G Veress needle, and 3mm laparoscopic trocar conducted in a positive pressure ventilation tension hemopneumothorax model using anesthetized swine. Susceptibility to tension physiology was extrapolated from volume of carbon dioxide (CO2) instilled and time required to induce 50% reduction in cardiac output. Failures to rescue and recover were compared between the 10% and 20% estimated blood volume (EBV) HTX groups and across devices. Results: A total of 196 tension hemopneumothorax events were evaluated. No differences were noted in the volume of CO2 instilled nor time to tension physiology. HTX with 10% EBV had fewer failures compared with 20% HTX (7% versus 23%; p = .002). For larger-caliber devices, there was no difference between HTX groups, whereas smaller-caliber devices had more failures and longer time to rescue with increased HTX volume as well as increased variability in times to rescue in both HTX volume groups. Conclusion: Increased HTX volume did not predispose tension physiology; however, smaller-caliber devices were associated with more failures and longer times to rescue in 20% HTX as compared with 10% HTX. Use of larger devices for decompression has benefit and further study with more profound hemorrhage and HTX and spontaneous breathing models is warranted.